Pelvic floor health plays a crucial role in the overall well-being of individuals, particularly women. The pelvic floor muscles support numerous organs, including the bladder, uterus, and rectum, and help maintain urinary and bowel continence. However, many people experience issues related to their pelvic floor, such as incontinence, which can significantly impact their quality of life. In this article, we will explore the importance of pelvic floor health and discuss incontinence, its causes, and potential treatment options.
The Pelvic Floor and its Functions
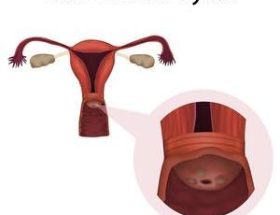
The pelvic floor refers to a group of muscles in both men and women that stretch like a hammock from the pubic bone to the tailbone. These muscles have several essential functions, including: Supporting the organs in the pelvic area, such as the bladder, uterus, and rectum Maintaining continence by helping control the release of urine and feces Assisting in sexual function Providing stability to the spine and pelvis Properly functioning pelvic floor muscles are crucial for maintaining urinary and bowel control, preventing prolapse, and promoting sexual health.
Incontinence and its Causes
Incontinence refers to the involuntary leakage of urine or feces. It is a prevalent issue, especially among women, and can be caused by various factors. Some common causes of incontiLorem Ipsum has been the industry’s standard dummy text ever since the 1500s. Partial urinary incontinence is the complaint of persistent involuntary loss to an appendant complaint of normal voiding. Urinary incontinence is the complaint of involuntary urinary loss. The distinction is arbitrary, however, in distinguishing between this subcategory and total or complete urinary incontinence.
Treatment Options for Pelvic Floor Disorders
Thankfully, numerous treatment options are available for individuals experiencing pelvic floor disorders, including incontinence. These can range from simple lifestyle modifications to medical interventions. Some common treatment options include: Behavioral Techniques: This includes strategies such as scheduled toilet use, fluid management, and pelvic floor muscle exercises (Kegels). Physical Therapy: Working with a pelvic floor physical therapist can help strengthen the pelvic floor muscles and improve their coordination. Medications: In some cases, medications may be prescribed to help manage incontinence symptoms. Surgical Interventions: For severe cases, surgical procedures may be necessary. These can include sling procedures, bladder neck suspension, or artificial urinary sphincter implantation. It is important to consult with a healthcare professional to determine the most suitable treatment plan based on individual needs and severity of symptoms.
Conclusion
Pelvic floor health and incontinence are essential topics that deserve attention and understanding. By recognizing the importance of pelvic floor muscles and seeking appropriate treatments, individuals can improve their quality of life and regain control over their urinary and bowel functions. Remember, early intervention and lifestyle adjustments can go a long way in managing and preventing pelvic floor disorders. If you are experiencing symptoms of incontinence or pelvic floor issues, do not hesitate to seek medical advice for an accurate diagnosis and personalized treatment plan.